Clockwise from top left: Roger Greenhalgh (London, UK), Stéphan Haulon (Paris, France), Gustavo Oderich (Rochester, USA), Nikolaos Tsilimparis (Munich, Germany), Bijan Modarai (London, UK) and Said Abisi (London, UK). Click on the image to watch the Juxtarenal Aneursym Consesus session on demand.
During the last five weeks, CX 2020 LIVE has attracted over 6,000 registrants from more than 120 countries. The topic of the 10th and final session was Juxtarenal Aneurysm Consensus. Experts covered cutting-edge developments in the field and tips and tricks for complex procedures. They also examined outcomes with a range of devices on the market. There was lively discussion reviewing surgeon-modified and custom-made fenestrated endografts and strong support for inner branch technology, backed by 79% of participants. Other topics covered include bridging stent grafts, balloon-expandable covered bridging stents, and off-the-shelf solutions for hostile necks. The session was chaired by Stéphan Haulon (Paris, France) and moderated by Gustavo Oderich (Rochester, USA), who cautioned against being a staunch defender of one technique over another, as “everything has a potential role”.
Said Abisi (London, UK) reported on experience with inner branch technologies and noted that although endovascular aneurysm repair (EVAR) and branched endovascular aneurysm repair (BEVAR have “good outcomes”, they are limited by “certain anatomical challenges which can make these procedures difficult”. Fenestrated procedures in particular require “very accurate planning and positioning”, and vessel deformation due to infrarenal angulation and iliac tortuosity may result in “unpredictable outcomes”, he adds. In addition, traditional BEVAR with outer branches “requires enough working lumen for the branches to open out and also requires long aortic coverage and a longer distance for bridging stents”.
The researchers set out to examine a cohort of patients undergoing fenestrated and branched EVAR over the past two years, focusing on procedural outcomes to investigate the indications for use of inner branches.
Abisi summarised that inner branches “have a good early outcome for the treatment of highly complex aortic aneurysms”, adding that they are “easy to use, adaptable to variable anatomy, and have demonstrable advantages compared to conventional technology”. However, he noted that longer-term data are needed to determine their wider applicability.
Responding to a question from Oderich regarding patency concerns, Abisi outlined that “this is why we are currently very cautious about selecting only those who are not suitable for standard fenestrated or branched”, and concluded that, as a result, the data need to be monitored, with patients followed-up over the long term.
Tips and tricks for repairing a thoracoabdominal aortic aneurysm using an off-the-shelf device
Bijan Modarai (London, UK) presented a case that demonstrated the repair of a large thoracoabdominal aortic aneurysm using an off-the-shelf thoracoabdominal branched device. The Zenith t-Branch (Cook Medical) incorporates four downward-facing outer branches and is designed to be coupled in a modular fashion with proximal and distal components to allow treatment of a variety of aortic anatomies. Modarai noted that “a number of markers on the stent graft facilitate accurate positioning, once it is placed inside the aorta”. He described the techniques adopted, which ultimately led to successful sealing of the aneurysm.
Asked about what the best strategy is for preventing bridging stent failure, Modarai answered that “the mode of failure is multifactorial. I do not think it is about saying whether it is best to use a balloon-expandable or self-expandable stent. I think it comes down to good quality control”. He went on to explain that this means “adequate sizing; ensuring that those branches are positioned in the optimal way so that the bridging distance is not very long; ensuring that the stent is [far] enough inside the branch so that there is adequate overlap, and to make sure that the stent is not too far deep into the target vessel”.
In regards to the use of antiplatelet therapy, Modarai stated that because “we do not have level one evidence, I tend to put these patients for at least a year, if not for life, on dual antiplatelet agents in the hope that all of those measures will reduce the chances of a stent occlusion” but commented that a “mistake” that a lot of people make is to compare branches with fenestrations, which he said is “like comparing apples with oranges”.
A further question on the spinal complication rate, which Modarai highlighted was “the most feared complication with these repairs”, and how best to prevent it, led Modarai to remark that the rate of cord complication is “related to the amount of the aorta that is covered”. In terms of prevention, Modarai asserted that “again, I think it is multifactorial; some of the repairs are worth staging”.
Custom-made fenestrated endografts are “first source” for elective repair, but surgeon modification useful in emergencies
Nikolaos Tsilimparis (Munich, Germany) offered an insight into the technical success achieved through surgeon-modified fenestrated endografts compared to custom-made fenestrated endografts. His presentation revealed that surgeon-modified endografts have been associated with higher type 3 endoleaks and reintervention, but achieve similar long-term outcomes to the custom-made devices.
However, Tsilimparis noted that to directly measure up the two treatment options side-by-side could be seen as an “unfair comparison”, commenting that they are “two different entities”. In particular, he highlighted the role physician-modified endografts have to play in urgent aortic repairs, adding that custom-made devices should be seen as the “first source” for elective repair. This conclusion was echoed by Oderich who commented that he had raised “a very important point, which is that sometimes you are in a tight spot where you cannot use an off the shelf device, or, it is not in the best interests of the patient”.
Oderich asked Tsilimparis for his thoughts on the importance of gaining experience with FEVAR in general, and the importance of quality control in modifying a device, particularly with regard to sizing and planning. Tsilimparis commented that many surgeons had made the mistake of trying to learn the fenestrated endograft technique and how to modify the device simultaneously, rather than opting to use custom-made devices initially. “This is a big challenge when you try to do both at once,” Tsilimparis added. “It is important in my eyes to start with easy cases with custom-made devices, and really rely on surgeon-modified [devices] if you have the experience with these, and also if you feel very comfortable with the stent grafts and the technique overall.”
An audience member from India asked Tsilimparis why he felt there was a higher rate of type 3 endoleaks seen in surgeon-modified, compared to custom-made devices. Tsilimparis replied that there were “some technical aspects” to explain this disparity, including some differences in sealing techniques between both device types. He also commented that, often, surgeon-modified endografts may be used in cases where there is a further distance between the aortic wall to the stent graft, citing this as another possible cause.
“New generation” of bridging stent grafts addresses flexibility and deliverability
Following Tsilimparis, Eric Verhoeven (Nuremberg, Germany) then detailed his centre’s experience of the use of a “new generation of bridging stent grafts”—the BeGraft and BeGraft+ (Bentley), the former for use in fenestrations, and the latter in branched procedures. Verhoeven told the CX 2020 LIVE audience that these latest devices have a higher radial force than earlier generations, as well as an increased kink resistance.
Summarising his experience, Verhoeven welcomed the development of the “new generation” devices. He added: “The transition with the target vessel is something to watch and sometimes you have to reline, and sometimes extend with a self-expandable stent to smoothen the transition zone.”
In the discussion following Verhoeven’s presentation, Haulon remarked that he was “surprised to see that everyone today is using balloon-expandable stents”, to which Oderich concurred, adding “and I think that reflects significant improvementby the industry to address the issue of flexibility of these stents and deliverability through a small profile”.
CX 2020 LIVE audience show strong support for inner branched technology, but more data needed
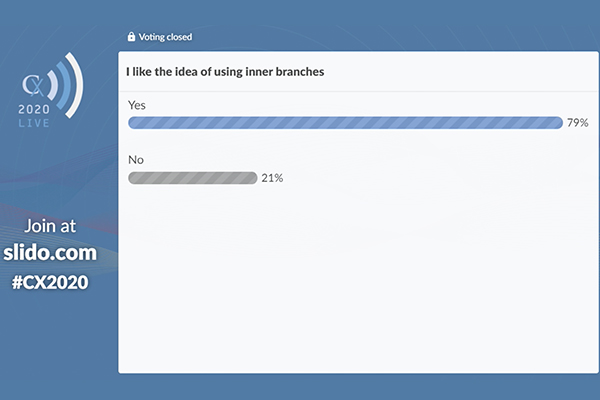
Polling half way through proceedings revealed that 79% of the audience like the idea of using inner branched technology, with Haulon commenting: “It seems that everyone believes that it is an interesting idea to use inner branches, so we need to evaluate those and hopefully we will have data to support the use of this new design in the near future.”
Best balloon-expandable covered bridging stent depends on surgeon preference, target artery anatomy
Mauro Gargiulo (Bologna, Italy) compared a range of balloon-expandable covered bridging stents (BECS) for fenestrated and branched endovascular aneurysm repair procedures.
On the current indications for using BECS for fenestration, Gargiulo stated: “All of us agree that the balloon-expandable stent graft is the choice, according to long-term results reported in the literature”.
Regarding branched procedures, Gargiulo noted that while some literature indicates no difference in occlusion or reintervention comparing balloon-expandable and self-expandable stents, other work favours the self-expandable graft for these procedures.

Clockwise from top left: Roger Greenhalgh (London, UK), Stéphan Haulon (Paris, France), Gustavo Oderich (Rochester, USA), Jean-Paul de Vries (Groningen, Netherlands), Mauro Gargiulo (Bologna, Italy), Eric Verhoeven (Nuremberg, Germany).
“In our centre, we use a balloon-expandable stent graft in all target artery anatomy expect renal arteries type B and D,” Gargiulo reported, adding that a hybrid approach, with a self-expandable balloon distally and a balloon-expandable stent proximally results in an increase of renal artery patency and is a good option for type B and type D renal arteries.
Gargiulo then listed ideal features of a stent graft, including navigability, visibility, precise deployment, conformability, radial force, flaring attitude, and patency.
Considering the structural features and biomechanical properties of various devices on the market, Gargiulo summarised: “The advantages of the iCAST/V12 [Getinge] are the precise deployment and the proven long-term results; the BeGraft , its good trackability, high flexibility, and the compatibility with the 6Fr sheath; and the VBX [Gore], its high flexibility, heparin-bonded bioactive surface, good trackability, and wide range of lengths.”
“I do not think there is a best BECS for all occasions,” Gargiulo concluded. He detailed that for fenestration, surgeon preference, the aortic endograft device, and the target artery anatomy are all important factors, and for branched procedures, the surgeon’s preference, the cannulation of the branch from either brachial or femoral access, and the target artery anatomy are key.
Off-the-shelf endovascular solutions for the treatment of AAAs with a hostile neck
Jean-Paul de Vries (Groningen, the Netherlands) told the CX 2020 LIVE audience how to achieve durability with off-the-shelf solutions for the treatment of abdominal aortic aneurysms (AAAs) with a hostile neck while minimising hospital resource impact.
By evaluating the seal zone of the three types of aortic necks—adequate, hostile, and inadequate—one can isolate the different needs in those necks and patients, de Vries noted.
He stated that, for the adequate neck, you only need seal, whereas in the hostile neck, you need additional strength, and in the inadequate neck, you need also to extend the seal to the juxtarenal or suprarenal aorta.
He recommended using the “gold standard” of endovascular aneurysm repair (EVAR) when there is an adequate seal zone, endosuture aneurysm repair (ESAR) in hostile necks , and a fenestrated or chimney device in an inadequate neck. “With a chimney device, the advantage is there is no waiting time, it is off-the-shelf, and the total costs are lower compared to fenestrated devices. However, it is limited to a maximum of two chimneys,” de Vries told the audience.