Clockwise from top left: Roger Greenhalgh (London, UK), Hugh Markus (Cambridge, UK), Ross Naylor (Leicester, UK), Peter Schneider (Honolulu, USA), Andrew Clifton (London, UK) and Lars Lönn (Copenhagen, Denmark).
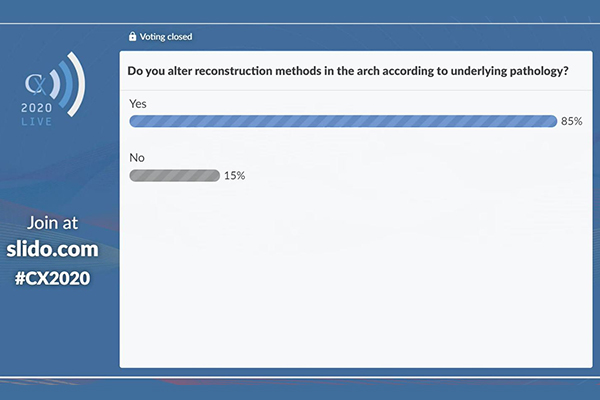
Over 6,000 registrants from more than 120 countries have signed up to participate in CX 2020 LIVE to date. The penultimate session, focusing on acute stroke, sought to find consensus on some of the thorniest issues of the day, yet discussion yielded the closest polling results of the live event so far. A presentation on the benefits of simultaneous surgical carotid and coronary artery revascularisation split opinion, and attendees heard of the “huge” global variation in carotid surgery. Furthermore, the optimal medical therapy for patients with bilateral stenosis, including the potential place for novel oral anticoagulants (NOACs), was examined, and promising technologies such as transcarotid artery revascularisation (TCAR), intracranial stenting, and virtual simulation were put under the spotlight.
As CX chair, Roger Greenhalgh (London, UK) introduced session chair Hugh Markus (Cambridge, UK) chaired the session and moderator Ross Naylor (Leicester, UK), who took live questions from participants joining the session from 62 countries.
Debate surrounding simultaneous versus staged surgical carotid and coronary artery revascularisation remains unresolved
Barbara Rantner (Munich, Germany) presented the argument that when performing carotid endarterectomy in a patient undergoing a coronary artery bypass graft (CABG), the two procedures should be done simultaneously. The question at the heart of her presentation was whether it is best to group all the surgical risks associated with procedures to avoid stroke and death, or whether to stagger them.
Consensus from the CX 2020 LIVE audience was lacking: 53% of polling respondents disagreed with Rantner’s premise that carotid artery revascularisation should be performed at the same time as coronary artery revascularisation, while 47% agreed.
“There is a clear indication for carotid revascularisation in recently symptomatic patients, and in asymptomatic patients with severe bilateral stenosis or higher latent stroke risk from a unilateral stenosis,” Rantner concluded. “The literature shows that stroke and death rates are comparable for combined and staged surgeries. Cardiac complications, and thereby overall procedural complications, are however higher amongst patients undergoing a staged surgical approach. We shall bear in mind that staged carotid artery stenting, especially in the last few years, has shown promising results amongst those patients.”
However, Naylor said that simultaneous carotid and coronary artery revascularisation has been “controversial” for decades, adding that the debate is not yet resolved.
An attendee from Moldova asked: “Can we say that indications for carotid revascularisation are independent from the need of CABG?”, prompting Rantner to reply: “Yes, I think that might be the goal. Especially for asymptomatic patients, that is still more important.”
International variation in carotid surgery is “huge” despite all the randomised trials performed
Maarit Venermo (Helsinki, Finland) shared what Markus (Cambridge, UK) referred to as “some very dramatic figures” from the International Consortium of Vascular Registries (ICVR), a collaboration formed in 2014 between the US Food and Drug Administration (FDA) Medical Device Epidemiology Network, the Society for Vascular Surgery (SVS)’s Vascular Qualities Initiative (VQI), and the European Society of Vascular Surgery (ESVS)’s Vascunet.
“Despite significant evidence on the treatment of carotid artery disease, there is large international and national variation in the proportion of asymptomatic patients, the proportion of octogenarians, the gender distribution, and the utilisation of carotid artery stenting,” Venermo relayed.
She continued: “This seems to be influenced by reimbursement systems, [which are different in each country]. Guidelines are also different, as is the interpretation of the carotid studies; collaboration between the guideline committees would be crucial to harmonise the treatment. Registry collaborations spanning the globe, such as ICVR, can provide important data to inform and unify best practices and treatment guidelines.”
During the discussion that followed Venermo’s presentation, several audience members asked after the variation in the proportion of octogenarians undergoing carotid surgery between countries. Overall, this varied from 0–20%, with the variation being higher in asymptomatic patients. Finland, Sweden, and Switzerland had the lower proportion of octogenarians undergoing carotid surgery, and Australia, Italy, and the USA had the highest.
Speaking specifically about this older cohort of patients, Venermo responded to questioners asking why she believed such a high proportion of patients around the world over 75 are being offered endarterectomy: “We had quite a lively discussion with the vascular surgeons in the USA,” she said. “They did not see this age question as at all as restrictive as saw it in Europe, especially in the Nordic countries, where we really stick to the 75 years of age [maximum], and even have a little bit of a lower threshold for women. But I think that the answer to this question is different in the USA to, for example, Italy.”
This was touched on by Mehmet Kurtoglu, tuning in from Turkey, who asked why the proportion of octogenarians being treated was higher in the USA. “I think that the whole healthcare system is different,” Venermo replied. “The USA has a system where you have individual patients, and maybe you have some motivation from your private interests. I would also say that I do not believe that we should not perform new carotid endarterectomies to asymptomatic patients. I think that if they do that, we leave some patients out of the procedure who really would benefit from it.”
Bilateral carotid stenosis patients may be an ideal cohort for intensive medical therapy with novel agents
Patients with asymptomatic bilateral carotid artery stenosis, Dominic Howard (Oxford, UK) reported, represent a high-risk group and may be suitable candidates for newer therapies—such as novel oral anticoagulants (NOACS)—in additional to standard medical therapy. Howard explained that the aim with these patients is to “maximise their protection against cardiovascular risk”. “They are at much higher risk of having a myocardial infarction than they are of having a stroke,” he added. Therefore, all treatments can be considered, even if data have to be extrapolated from other areas.
Howard outlined data from the Oxford Vascular Study (set up by Peter Rothwell in 2002), which is a prospective population-based study of medically-treated patients with asymptomatic carotid stenosis. Results show that, compared with patients with unilateral disease, those with bilateral disease have a significantly lower rate of freedom from cardiovascular events at five years. They also have a significantly lower rate of freedom from cardiovascular death. “Patients with bilateral carotid artery disease do appear to be a very high-risk group and may be an ideal cohort to treat with intensive medical therapy and potential novel agents to reduce death and disability,” he observed.
In the discussion following Howard’s presentation there was another question from Kurtoglu, who asked if such therapy should include NOACs. Howard responded that the COMPASS trial suggested that a NOAC (plus aspirin) may be appropriate for patients with bilateral carotid artery stenosis (depending on their individual characteristics). He explained that both the COMPASS trial and the FOURIER trial were “interesting” because they showed that newer agents (a NOAC and a PCSK9 inhibitor, respectively) could reduce cardiovascular events in patients with vascular disease. Furthermore, Howard suggested dual antiplatelet therapy might be an option, but noted that this was “a personal opinion because there really is not any [specific] data out there”. “They [patients with bilateral disease] are certainly a group that need to have everything thrown at them because they are very high-risk cohort,” he observed.

Clockwise from top left: Roger Greenhalgh (London, UK), Hugh Markus (Cambridge, UK), Ross Naylor (Leicester, UK), Peter Schneider (San Francisco, USA), Andrew Clifton (London, UK) and Lars Lönn (Copenhagen, Denmark).
More data needed for TCAR
Peter Schneider (San Francisco, USA) reviewed the latest data for transcarotid artery revascularisation (TCAR, Silk Road Medical), which he said had shown comparable rates of stroke/death to carotid endarterectomy. However, he also acknowledged that key data for the procedure, such as outcomes for when TCAR is performed within seven to 14 days of symptom onset, are lacking and that further trials are needed.
He told the CX 2020 LIVE audience that transfemoral carotid artery stenting is associated with an increased rate of diffusion-weighted magnetic resonance imaging (DW-MRI) lesions: 70% vs. 17% for patients who have undergone carotid endarterectomy. Furthermore, Schneider commented, the stroke rate following transfemoral stenting is of “particular concern”.
However, he said that TCAR was a “possible path forward for carotid stenting”—explaining that it involved “the use of a proximal clamp on the common carotid artery with flow reversal and a circuit to the femoral vein”. “This permits avoidance of the arch, the ability to use proximal protection, protection of the brain prior to crossing, improved particle capture, and the ability to back flush (which we do with carotid endarterectomy),” he added.
Schneider reported that studies have shown that TCAR is associated with a low rate of stroke/death. In particular, it has lower rates of stroke/death than transfemoral stenting and comparable rates to surgery. Specifically, data indicate no significant differences in the rate of stroke/death between TCAR and carotid endarterectomy in symptomatic patients. He further observed that Parakevas et al conclude that TCAR has “a high technical success rate, almost zero mortality, and very low major/minor stroke, myocardial infarction, and complication rates”.
However, in the discussion following Schneider’s talk, Naylor commented that no data were available for “stroke/death stratified by when TCAR is performed within seven to 14 days of symptom onset, which is now the gold standard for carotid interventions for patients around the world”. Schneider accepted that this “needs to be addressed”, noting a prospective study investigating early TCAR is underway.
Intracranial stenting and advances in simulation
Arguing that “intracranial stenting for stenosis is not dead”, Andrew Clifton (London, UK) compared results from the SAMMPRIS trial, which did not favour stenting with the WingSpan device (Boston Scientific), and the WEAVE trial to refute the “traditional dogma” that best medical treatment should be the favoured approach.
Clifton outlined the limitations of the SAMMPRIS trial, with specific reference to the minimum requirement of operator experience. “A minimum of three WingSpan stent cases were required for the operators. It is, if you have not used it, quite a complicated device,” he said.
This is in contrast, he explained, to the WingSpan stent system post-market surveillance (WEAVE) trial, where interventionalists were “required to be genuinely experienced”. He highlighted that operators with greater than 50 WingSpan cases before enrolment in WEAVE had a 0% (out of 69) periprocedural stroke and death rate.
Thus, Clifton proposed that findings from WEAVE indicate that the poor clinical outcomes observed in SAMMPRIS were not necessarily due to the stent, but more likely due to the inexperience of the interventionalists, as well as poor patient selection and underdeveloped standards in intracranial stenting. “We need to proceed to a careful randomised controlled trial,” he told the CX 2020 LIVE audience.
The discussion saw Naylor question the relevance of such a trial when a more generalisable set of interventionalists will have to perform the procedures in the long run.
Clifton replied: “When you are looking at a patient who has had a stroke, particularly the subsets—Afro-Caribbean or Asian—that have a high incidence of intracranial stenosis, you need to select them carefully [and] perhaps refer them on to a centre that does a lot of these; not every centre should do them.”
Clarifying that the technology and medical treatment have improved since the SAMMPRIS trial, Clifton reiterated: “The centre’s experience is very important when it comes to managing these patients, as is the experience of the interventionalist (usually a neurointerventionalist), who has got the numbers under their belt, and the audit to prove they can do it safely.”
On the subject of ensuring the safety of stroke procedures, Lars Lönn (Copenhagen, Denmark) discussed validation studies of virtual reality simulation performance metrics for mechanical thrombectomy.
“Despite the proven effectiveness [of mechanical thrombectomy],” he began, “access is limited, and one of the reasons is a shortage of operators trained for the procedure. One approach is to enhance the learning experience and train doctors to do the procedure using metric-based virtual simulation.”
A group of senior interventional experts at the ASSERT centre, University College Cork, Cork, Ireland, in conjunction with Mentice, have created the training simulation method. “We set out to determine whether a simulator could distinguish between novice interventional neuroradiologists and experts,” he explained. The team found that experienced practitioners, when compared to “rookies”, were 47% faster and had 97% fewer errors.
During the discussion session that followed, Naylor queried whether Lönn’s team has considered training consultant cardiologists or physicians from other disciplines to do mechanical thrombectomy, given the shortage of neurointerventionists.
Refusing to be drawn into the politics around specialty, Lönn replied: “A proctor in the simulator gives you tips and tricks in a structured way, so you train everyone in the same manner, which is a good thing. We can also test this to see if they have reached a certain level. If they have, then of course they have proficiency, regardless of their initial speciality. But they have to train.”
An incoming question from Argentina touched on whether stimulation should be obligatory in training programmes. Clifton shared his “strong opinions on this”, arguing that stimulation is a great adjunct, but not a replacement for traditional apprenticeships. Lönn agreed: “The apprenticeship model cannot stand alone, and simulation cannot stand alone.”
Greenhalgh noted that voting from CX 2019 supported the belief that, as long as adequate training was undertaken, the interventionalist need not be a neuroradiologist. The debate on whether neuroradiology training is a prerequisite for performing stroke interventions therefore prevails.