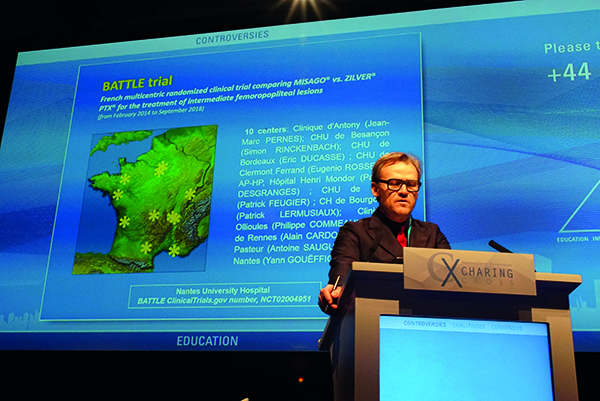
Yann Gouëffic
The BATTLE trial comparing a drug-eluting stent (Zilver PTX, Cook) vs. a bare metal stent (Misago, Terumo) for the treatment of intermediate femoropopliteal lesions has failed to the show superiority of the paclitaxel-coated stent at one-year follow-up. The trial highlights a need for further direct comparative data between devices and strategies for treatment of femoropopliteal lesions.
The data were presented for the first time by Yann Gouëffic (Nantes, France). BATTLE is a French multicentre randomised clinical trial including 10 centres and 181 patients, randomised 1:1 into the Misago bare metal and the Zilver PTX drug-eluting stent arms (n=85 vs. n=86, respectively). At one year, 78 and 82 patients completed follow-up, respectively. Included patients were classed as Rutherford 2–5, with de novo atherosclerotic femoropopliteal lesions of 2–14cm and a reference vessel diameter of 4–7mm.
There are currently several different options for treating TASC A and B lesions, Gouëffic said, including bare metal stents, drug-eluting stent, drug-coated balloons and covered stents. However, few head-to-head randomised trials have been completed so far to compare the safety and efficacy of devices for femoropopliteal lesion treatment. Instead, the hypothesis for the BATTLE trial was formed of indirect data from comparative trials of bare metal stents vs. percutaneous transluminal angioplasty (PTA) with a non-coated balloon. Data from the Zilver PTX randomised controlled trial indicated that the paclitaxel-coated Zilver PTX fared better compared to bare metal stent. This comparative data from a second arm of randomization of Zilver ptx trial, Gouëffic explained, led to the hypothesis that Zilver PTX would prove superior to the bare metal Misago stent and subsequently the BATTLE trial was designed as a superiority trial, rather than non-inferiority.
The patient population at baseline showed similar mean lesion lengths and reference vessel diameters, with intermittent claudication present in 82% and 79% of patients in the Misago and Zilver PTX arms, respectively. There were no significant difference in procedural characteristics in term of pre- and post-dilation but the mean stent lenght. Technical success was 100% in both arms.
At 12 months the primary endpoint—freedom from in-stent restenosis—was 85.7% in the bare metal stent arm, and 90.3% in the paclitaxel-eluting stent arm (p=0.36). The primary endpoint was defined by restenosis of >50%, as well as a peak systolic velocity index of >2.4 at the target lesion.
Secondary endpoints, however, showed a marked lack of significant superiority in the paclitaxel-eluting stent arm. Patency rate was 81.6% vs. 84.2% (p=0.41) for Misago and Zilver PTX, respectively; target extremity revascularisation was 3.8% vs. 4.9% (p=0.52) and notably, target-lesion revascularisation was at 8.9% vs. 8.8% (p=0.91) respectively at 12 months. No difference was seen in Rutherford stage at baseline or at 12 months. Finally, there was an 85.3% clinical improvement in the bare-metal stent arm vs. 88.6% for Zilver PTX (p=0.56).
Due to the design of the study, Gouëffic explains they were not able to look at non-inferiority of the Misago stent, as opposed to superiority of the Zilver PTX. “This conclusion is not for all drug-eluting stents”, Gouëffic pointed out, as future generation devices may cause the field to change. “Advantages of drug-eluting therapy in comparison to bare metal stents are still required, to define the strategy for the treatment of intermediate length femoropopliteal lesions”, Gouëffic concluded.