Ulf Teichgraeber
The 12-month results from the full clinical cohort of the EffPAC randomised controlled trial, were presented for the first time at the CX Symposium yesterday.
Target lesion revascularisation at 12 months was 1.3% (vs 17.7% in the plain angioplasty group, p<0.001). Primary patency at 12 months was 90.3% (vs. 65.3% in the plain angioplasty group, p<0.001). Rutherford stage improvement at 12 months was 90.6% in the Luminor group (p=0.006), Teichgraeber reported. Ulf Teichgraeber (Jena, Germany) reported the 12-month outcomes of the Luminor paclitaxel-coated balloon (iVascular) for the treatment of superficial femoral and popliteal arteries. At 12 months, Teichgraeber noted that patency was significantly higher in patients who received drug-coated balloon therapy compared with those who received treatment with an uncoated balloon.
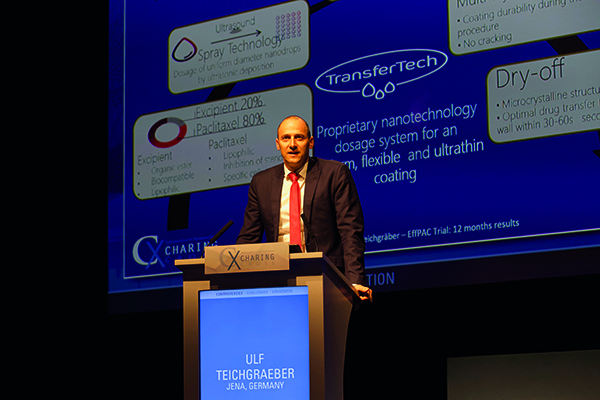
“What is special about Luminor drug-coated balloon, is its unique nano-coating technology, which is ultra-thin and uniform,” commented Teichgraeber, principal investigator of the study.
According to Teichgraeber, Luminor was not “just another” paclitaxel-coated balloon. As he explained it had a unique “nanotechnology coating”. “It is multilayer technology, which makes it seem very rigid. So, you may think: ‘how does paclitaxel get off the balloon?’ But, it increases adhesion to the balloon, improves durability, improves mechanical properties, and provides fast absorption (30–60 seconds)”.
The aim of the EffPAC trial, Teichgraeber commented, was to review how the device compared with an uncoated balloon. Patients with lesions in the superficial femoral artery or in the popliteal artery were randomised to receive treatment with Luminor (n=85) or with an uncoated balloon (n=86). So as to include as many people as possible in the trial, prolonged percutaneous transluminal angioplasty with the same balloon was performed in cases of non-flow limiting or flow-limiting dissection (in both groups). The primary endpoint was late lumen loss at six months, with secondary endpoints including freedom from target vessel revscularisation, patency, change in ankle-brachial index, Rutherford stage, and quality of life.
At 12 months, data were available for 76 patients in the Luminor arm and for 75 patients in the uncoated balloon arm. Teichgraeber noted that, at six months, the late lumen loss was 0.14mm for Luminor vs. 1.06 for uncoated balloon (p<0.01). However, he commented that this was “a technical endpoint” and the focus should be on clinical endpoint. “You might say it is target lesion revascularisation or patency that are most important, but I think it is more about assessing the benefit for the patient. And, therefore, the clinical result is the change in the Rutherford score,” Teichgraeber added.
He said “what was astonishing for us as investigators” was that there was strong evidence that Luminor was associated with an improvement in the Rutherford classification “not only compared with baseline levels but also with the uncoated balloon”. For example, at 12 months, 49.3% of patients in the Luminor group had an improvement of three stages compared with only 29.2% of patients in the uncoated balloon group. Furthermore, both the rate of target lesion revascularisation and patency were better with the drug-coated balloon.
Teichgraeber concluded: “The Lumnior paclitaxel-coated balloon catheter was demonstrated to be highly clinically effective and safe in inhibiting restenosis compared to an uncoated balloon. The innovation coating technology matters and is shown not only in the patency, late lumen loss, and target lesion revascularisation data but also in an improvement in the Rutherford classification. The results of the study allow direct comparison to other already-completed randomised controlled trials applying paclitaxel-coated balloon from different manufacturers to the same target vessel.”







