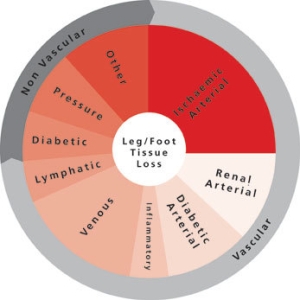
With the aim to promote the best possible care of the ischaemic lower limb to reduce the number of major amputations, the CX ilegx Collaboration Day will offer delegates an overview of the latest treatment strategies, particularly in patients with diabetes, one of the main causes of amputations.
This year, ilegx will address the reasons why amputations still occur in 2016 and discuss recent advances in care to prevent them including the interdisciplinary and rapid foot referral approach of the King’s College Hospital open access vascular diabetic foot care pathway as well as the latest developments for ulcer and wound healing treatment. Revascularisation strategies with updates on the BASIL-2 and 3 trials and BEST-CLI trial will also be presented and discussions on the topic “To stent or not to stent – that is the question” will be a highlight of this session.
Michael Edmonds (King’s College Hospital, London, UK), who is one of the founders of ilegx and co-director of the CX ilegx Collaboration Day course, gives insights on the importance of a proactive approach for diabetic foot treatment.

Michael Edmonds
What are the biggest challenges treating patients with peripheral arterial disease, particularly those with diabetes?
One of the biggest challenges is that diabetes has reached epidemic proportions and with it has come a growing number of complex lower limb problems including peripheral arterial disease, which is often accompanied by a peripheral neuropathy. Classical symptoms and signs of arterial disease such as claudication and rest pain may be absent because their expression depends on an intact peripheral nervous system. Thus, the traditional system in which a patient has a symptom, talks to his/her practitioner, and the practitioner makes a diagnosis and treats, is often not applicable to the patient with diabetes, vascular disease and neuropathy. Instead, there must be a meticulous assessment of the patient to look for subtle symptoms and signs of arterial disease, especially early skin breakdown, which is also very prone to infection. In the presence of peripheral neuropathy, the signs of infection, including pain and erythema, may also be severely diminished and practitioners should carefully inspect for early purulent discharge. Thus, all professionals looking after patients with diabetes and peripheral arterial disease should understand this atypical diabetic presentation of disease and adapt their clinical practice when treating these type of patients.
What are the most significant advances in diabetic foot treatment to reduce amputations?
There have been three crucial significant advances in diabetic foot care to improve the outlook of diabetic patients and to reduce amputations.
First, prompt diagnosis of ischaemia and urgent revascularisation below the knee and even below the ankle have been established as important aspects of the management of diabetic ischaemic feet. The critical factor in saving limbs is making a rapid diagnosis of ischaemia and administering the appropriate treatment early. In this way, speedy healing can be achieved and can prevent patients from undergoing needless amputations.
The second key advance has been the realisation that diabetic foot patients experience repeated crises from the rapid onset infection and need a special form of easily accessible care within an interdisciplinary diabetic foot service to provide prompt treatment of infection before it progresses to necrosis. Within such an interdisciplinary diabetic foot service, modern techniques in wound care and aggressive treatment of infection with surgical debridement and parenteral antibiotics are important.
The third advance has been the successful surgical reconstruction of deformed and unstable Charcot feet, even in the presence of treated peripheral arterial disease. This approach will be described in the CX ilegx Collaboration Day course.
The King’s College (London, UK) open access vascular diabetic foot care pathway—to be highlighted at ilegx—is an example of an interdisciplinary approach to save limbs; could you explain how it operates?
The diabetic foot can deteriorate with alarming speed and for this reason there is a need to offer a rapid and integrated service for diabetic foot patients. The King’s College open access vascular diabetic foot care pathway, through its diabetic foot clinic, provides open rapid access to accelerate urgent assessment and to proceed quickly to state-of-the-art interventions, including endovascular procedures, open vascular surgery, urgent surgical debridement and aggressive treatment of infection. The clinic is operated by an interdisciplinary team comprising surgeon, podiatrist, nurse, orthotist, radiologist and diabetologist.
What is the role of endovascular below-the-knee revascularisation in diabetic patients?
Endovascular revascularisation for the treatment of patients with below-the-knee peripheral arterial disease—including the plantar arteries—has developed considerably over the last decade. A growing number of centres favour an endovascular-first approach below the knee because of reduced morbidity and mortality compared with vascular surgery, nevertheless, having the surgical possibility as a backup if necessary. Endovascular revascularisation seems appealing as a first-line treatment as long as proper flow to the foot and ulcer area can be achieved.
What is the importance of wound healing in diabetic patients?
Whilst revascularisation is regarded as an effective treatment for ischaemia, poor wound healing rates have been described in the diabetic foot patient. Wound healing is a complex biological process. Whilst understanding of the process has increased rapidly in recent years accompanied by new adjuvant healing technologies, there are still many aspects of the normal healing process that are not completely worked out. As long as a foot ulcer or post-operative wound remains open, there is a considerable risk of infection in the patient with diabetes. Early closure of these lesions by split skin graft can be very successful.
Ilegx will have a special session titled “To stent or not to stent – that is the question” what are your views regarding this practice?
The arterial lesions in diabetic patients—particularly below the knee—are long, multilevel and multivessel. They are often occlusive and usually calcified; therefore, they are not especially suitable for stenting. The main reason for stenting in the lower limb of patients with diabetes is bailout stenting at sites of flow limiting arterial dissection.
Click here to read an overview of the highlights of the CX 2015 ilegx Collaboration Day
About ilegx
The ilegx initiative, launched in 2008, was created in response to the increasing number of lower limb amputations which are mostly due to type II diabetes.
ilegx is a collaboration of like-minded health professionals, patients and care workers who share the view that too many legs are amputated and many of these are completely unnecessary.
The ilegx mission is to attract attention and draw awareness to the need for an improvement in health care in order to lower unnecessary major amputation of legs.
The CX ilegx Collaboration Day will take place at the Charing Cross Symposium on Thursday 28 April – Pillar Hall Learning Centre, Olympia Grand, London, UK
Click here to see the CX ilegx Collaboration Day programme
Click here to see the CX Interactive Main Programme – Peripheral Arterial Challenges
Click here to register







